Obstructive Sleep Apnea (OSA)
What it is
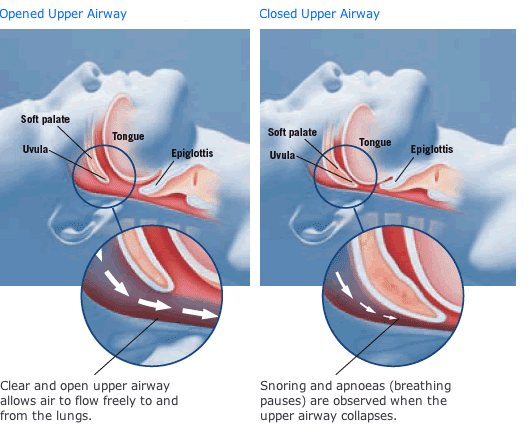
Obstructive sleep apnea (OSA) is medical condition occurring during sleep where relaxation of the oral musculature causes recurrent narrowing and/or collapse of the upper airway. This causes the individual to exert increased effort to breathe and have frequent micro-arousals throughout sleep to correct the pathology.
Misconceptions
OSA is a disease of the old and/or severely obese - FALSE! It is a disease of the bone structure of the face, and therefore you can be young and thin and still have OSA!
You have to be sleepy to have OSA - FALSE! According to the Wisconsin Cohort Sleep Study, only 37% of patients with severe OSA complain of excessive daytime sleepiness. So not only is sleepiness not a requirement, it occurs less than half the time!
The pathology of OSA stems from drops in oxygen during the night, which deprives your heart and brain of oxygen - PARTIALLY TRUE. The major pathology of OSA has to do with pressure dynamics in the chest (see “The Nuts & Bolts” below).
The Nuts & Bolts
OSA is a very common condition, affecting children to the elderly, males and females, people who are overweight and those who are at ideal body weight.
It is estimated that 80-85% of all people with OSA in the United States currently are undiagnosed.
Untreated OSA can increase the risk of stroke, heart attack, hypertension, heart dysrhythmias, diabetes, dementia, depression, anxiety, and many other medical ailments.
An explanation of the physiology (taken from Dr. Meskill’s 2/13/2015 article from the Huffington Post):
When a person goes to sleep, the body's muscles become more relaxed, including those of the jaw, the tongue, and the throat. This leads to the jaw and tongue sliding back, and the throat becoming less rigid. These changes make the diameter of the top of the airway narrower, requiring more effort to pull air into the lungs. This can lead to airflow turbulence, creating vibration of the soft tissue in the airway. This sometimes produces sound (i.e., snoring) and can lead to mucosal irritation and mucous production during the night. The body compensates for this airway narrowing by increasing chest expansion, which generates a stronger vacuum force in the chest to pull the air into the lungs. In OSA, the soft tissue at the top of the throat may collapse due to this vacuum, closing the airway.
However, the relatively narrow opening leads to sustained increased effort to breathe during the night. The body sometimes thrusts the jaw forward and clenches it in place in order to keep the tongue forward to widen the diameter of the top of the airway. This thrusting is the source of teeth grinding, while the clenching can lead to significant muscle soreness and headaches.
Meanwhile, the sustained increased respiratory effort to pull air through a narrower opening is interpreted as abnormal by the peripheral nervous system, leading to strong signals being sent to the brain that cause brief disruptions in sleep. These disruptions interrupt the normal sleep cycle, reducing the efficiency of the brain's restorative process and therefore can lead to daytime sleepiness and fatigue, as well as impaired concentration and memory.
The vacuum pressure generated in the chest also increases the work needed for the heart to contract, which can lead to a reduction in the amount of blood ejected from the heart. Over time, this can lead to mild swelling of the right side of the heart, which influences the heart to release factors into the bloodstream that signal the kidneys to waste fluid to reduce the volume entering the heart. This can lead to more frequent trips to the bathroom due to increased urine production.
This vacuum pressure also can lead to acid being pulled up from the stomach and into the esophagus, leading to heartburn at night. Certain stages of sleep (especially Rapid Eye Movement, or REM sleep) are more prone to airway restriction than others, and thus there may be predictable timing of awakenings during the night. The increased effort may lead to elevated heart rate and sweating, as well.
The Symptoms
Excessive daytime sleepiness (EDS) - EDS is sleepiness above and beyond “normal” and not due to behavioral causes (e.g., not getting enough sleep because you go to bed too late). Sleepiness is subjective by nature, so tools are used to help decide what’s “abnormal.” The most widely used tool is the Epworth Sleepiness Scale. Scores above 10 out of 24 are considered EDS.
Fragmented sleep - Fragmented sleep is a hallmark of many sleep disorders, but it is a common occurrence in OSA. Sometimes, this means the individual will wake up frequently during the night. Other times, it just means that sleep is highly disjointed at the level of the brain, but the individual does not wake up.
Morning jaw/TMJ discomfort - The medical term for clenching and/or grinding teeth is “bruxism.” Bruxism during sleep is a common trigger of TMJ pain. Quite often, the reason for sleep bruxism is sleep-disordered breathing (e.g., OSA).
Brain fog - Brain fog — that feeling like one’s mind is in a cloud and can’t function at full capacity — is a common symptom of poor sleep and a frequent complain of individuals with untreated OSA.
Nocturia - If you have to get up regularly at night to urinate, that’s called “nocturia.” Men often will attribute this to their prostates, but OSA can be the cause as well. One way to distinguish from this is to analyze the occurrence: (1) When you get up to urinate, is it difficult to initiate the stream? (2) Is there a sizable volume (vs. just a trickle)? If the answers are “no” and “yes,” respectively, then OSA should be considered.
Headaches - Frequent morning headaches require a neurologic assessment, as these can sometimes be a symptom of a brain tumor. Thankfully, much more often they are due to a more benign pathology. OSA can cause headaches in two ways: (1) The muscle tension and soreness from clenching the teeth at night (see morning jaw/TMJ discomfort above) can cause headaches. (2) The mismatch between oxygen and carbon dioxide caused by moderate-to-severe OSA leads to blood vessel dilation inside the skull, and the resulting pressure can trigger headaches.
GERD/acid reflux - The increased vacuum force generated in the chest to pull harder to get air also creates a pressure gradient between the chest (where the esophagus is) and the abdomen (where the stomach is). This vacuum in the chest can facilitate acid escaping the stomach and entering the esophagus, which is what causes acid reflux, or “heart burn.”
Dry mouth - Human beings are designed to breathe primarily through their noses. When nasal breathing is difficult (e.g., exercising), then oral breathing is our rescue/backup breathing. Since OSA is a condition of impaired airflow, it is accompanied by oral breathing in virtually all cases. Unlike our noses, which are designed to filter and humidify air, the oral cavity is not designed for sustained airflow. When sustained oral breathing occurs, the mucosa get dried out, and dry mouth occurs.
Night sweats - Night sweats can be the result of a variety of conditions, ranging from cancer to menopause to viral illness. However, they also are a common symptom of OSA. The frequent micro-arousals that occur due to OSA events are not peaceful - they are stress events. They are accompanied by the production of stress hormones (e.g. , cortisol, norepinephrine, epinephrine). Think about the last time you had a stressful thought or sudden worry, and even though you weren’t exercising you felt yourself begin to sweat. This is what is happening during the night with OSA, and as a result you wake up sweaty, even if the sleeping environment is not hot.